Unfortunate Financial Disarray for a Family from California After an Expensive Emergency Room Visit with Their Burned Infant
In a shocking turn of events, a California family found themselves entangled in a battle with insurance companies and medical providers after their newborn son, Brody, sustained severe burns in an accident.
The Accident and Hospitalisation
The incident occurred in October 2022 when a rice cooker fell off a kitchen counter, causing second-degree burns to the baby. Brody was rushed to a nearby hospital, but due to a lack of a burn unit and an unavailable ambulance, he was transferred to another facility via air ambulance.
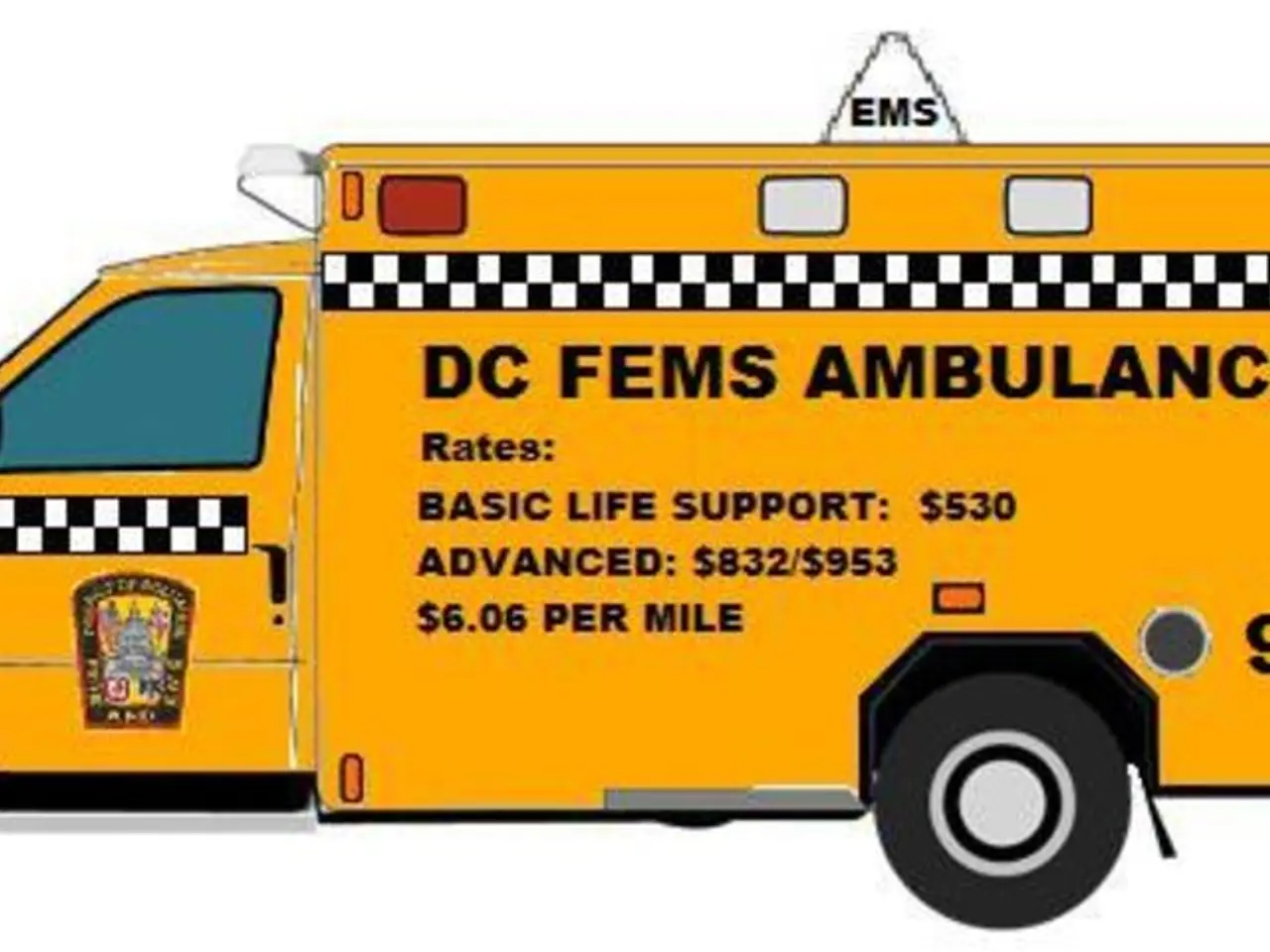
Upon arrival, an additional ambulance ride was required for a 0.3-mile distance, costing $10,200. Despite the emergency nature of the situation, Brody's insurance covered only a fraction of the ambulance bill, leaving his mother, Farwell, responsible for another $7,327.
The family's ordeal did not end there. They were forced to take a $90,000 air ambulance for a 15-minute ride to the hospital, a decision made necessary due to the lack of a suitable ground ambulance.
The Billing Conundrum
The family received bills totaling more than $100,000 for the helicopter ride and the ambulance ride. The bills included various fees such as a waiting fee and a fee for nighttime service. The $10,000 ambulance bill did not get waived initially because the transport took place in 2022, predating when the law that protects insured patients from surprise bills for ground ambulance services went into effect in January of last year.
Farwell made numerous attempts to resolve the bills with the hospital, ambulance company, and insurance but was met with no success. The situation was further complicated by the fact that the ambulance company, Pro Transport-1, and the insurance company seemed to point fingers at each other.
Legal Protections and Loopholes
California has laws to protect against surprise billing, but these protections do not extend to air ambulance services. The federal No Surprises Act, enacted in 2020, offers protection against surprise billing for emergency care and certain non-emergency services provided by out-of-network clinicians at in-network facilities. However, air ambulance services are not explicitly covered under the law's provisions for surprise billing protections.
In response to this gap in protection, California passed a law, AB 716, that protects consumers from surprise billing for ground ambulance services. However, the lack of federal coverage for air ambulances leaves patients like Farwell vulnerable to surprise bills.
Resolution and Advocacy
Investigative reporters and ABC's 7 On Your Side stepped in to help Farwell, getting both bills amounting to $100,032 waived. Pro Transport-1, the ambulance company, stated that the issue lies with the insurance company passing part of the bill to the patient, but they will accept their partial payment and no longer seek the remaining balance of the bill for their services.
Carmen Balber, executive director of Consumer Watchdog, expressed concern about the high cost of ambulance rides, especially for short distances. She advocates for more comprehensive laws to protect patients from such exorbitant bills.
As the story of Brody and his family unfolds, it serves as a reminder of the need for clearer regulations specifically addressing air ambulance services and the importance of advocacy in the face of unexpected medical bills.